The best glucose meters are handheld devices used to test your blood sugar levels at home. Glucometers enable you to get fast readings to see how diet, exercise, medication (such as insulin) and other factors affect your blood glucose. Because they’re a vital part of managing diabetes, glucose meters must be reliable, easy to use and as painless as possible.
While the cost of a glucometer won’t be covered by Medicare Part D plans, it should be covered by Medicare Part B (as Durable Medical Equipment). Choosing the best glucose meter for your needs is largely down to you, but your doctor may recommend which type of glucometer you’d benefit from. Standard glucose meters, for example, use a small lancing device that pricks your finger to collect blood for testing. These are the cheapest type of blood sugar monitor and the easiest for beginners to use.
We have consulted health experts and studied glucometer and blood sugar reading guidelines from health organizations including the CDC and WHO, as well as advice issued by the American Diabetes Association, and the American Association of Diabetes Educators. This guide is to aid your research, but we recommend speaking to your doctor about what type of meter is right for you.
Our promise to you
Continous Glucose Monitors (CGMs) are far more advanced. They monitor blood glucose levels day and night with little effort from you. CGMs store a greater amount of readings, but they are expensive and come with a learning curve. All of the best glucose meters below can store readings (numbers vary), with smart glucometers taking this up a notch. The latter will produce graphs (like CGMs do), showing you potential trends behind spikes and crashes. You’ll also get 30 to 120-day averages, plus a chance to add notes on diet, meds and activity.
When choosing the best glucose meter for you, do your research on the cost of compatible test strips. Hands-down, the ongoing cost of test strips will determine how expensive or cheap your glucometer really is. We’d advise speaking to your health insurance company to see what it will and won’t cover. Finally, if you have no or low vision, the best glucometer for you is one designed to speak results aloud, and we have included the top option for that type of monitor below.
What the Experts Say

According to advice published by the American Diabetes Association, blood sugar testing is vital to check that your blood glucose levels stay in a healthy range. ‘If glucose levels get too low, we can lose the ability to think and function normally. If they get too high and stay high, it can cause damage or complications to the body over the course of many years.’
To ensure you choose the best glucose meter for your needs, the American Association of Diabetes Educators recommends considering whether the following features are helpful to you:
- A high contrast display if you have low vision, or a meter that speaks results
- Lancet function and needle removal if you have a dexterity condition
- Portability for taking readings multiple times a day
- Smartphone app connectivity
- A bolus calculator (ability to assist with insulin dosage calculations)
- Approved for Alternate Site Testing
Susan Stauffer, BSN, RN, CDE, diabetes educator and nurse clinician at UCHealth Diabetes and Medical Nutrition Therapy in Fort Collins, Colorado, also highlights how insurance and the cost of test strips should factor in your decision: “The most important factor for people who routinely check their blood sugar is insurance coverage. Whether you use the Walmart Prime, the Freestyle lite or the Contour Next One, it is insurance coverage that rules. Some strips cost $18 for 100 and some will cost $150 for 100.”
Best glucose meter for smart diabetes management

The Ascensia Contour Next One Glucometer is designed to work with the Contour Diabetes smartphone app (iOS, Android), and has a five-second results countdown. You can program the glucose meter with alarms to remind you to check your blood sugar throughout the day, which is handy if you often forget, and there's a bright port light for increased visibility during testing.
One of the most useful features is the smartLIGHT target range indicator. This gives you instant visual (colored light) feedback by immediately recognizing if you blood glucose reading is above, below or within target range. This is one of the reasons why it's rated as one of the world's best glucose meters.
The Contour Next One has over 1,300 reviews on Amazon, with an average rating of 4.6 out of 5 stars. It scores 4.5 out of 5 stars on Walgreens, and from over 400 reviews on Walmart it has earned an average of 4.6 out of 5 stars. The large majority of reviews praise the high levels of accuracy, ease of use and the wealth of data captured, along with the easy-read display. Critical reviews are in the minority, with some users saying that the meter they used lost accuracy after a few weeks of use.
If you pair the Contour Next One with the Contour Diabetes app, readings will be stored for you to look through and pick out any trends. Pre- and post-meal blood sugar level reading results are saved, with Fasting, Before Meal, After Meal, and Overall results viewable on a daily graph.
The Contour Next One Glucometer presents averages over a 90-day period, and you can add in notes regarding diet, exercise and medication. This means you can not only see patterns, but the potential causes, enabling you to better manage your blood glucose day to day.
Another cool feature concerns the test strips, designed to enable Second-Chance sampling. This give you 60 seconds to reapply more blood, which could help prevent wasted strips if you didn't add enough blood for a reading the first time. The user manual goes into detail on all of these features, and includes information such as how to use the Contour Next One, and how to clean your glucometer.
- Read our Ascensia Contour Next One review
Best glucose meter for ketone readings too

The Fora 6 Connect glucose meter is popular among people who want to capture accurate blood glucose readings to see what foods and other factors spike their blood sugar, and could therefore help you make more informed nutritional choices to better manage your blood glucose levels.
An attractive aspect of the Fora 6 Connect is that it doubles as a ketone meter, and is one of few devices to do both types of monitoring effectively. It does so using two separate strips - one for glucose, one for ketones. A box of 50 Blood Glucose Test Strips costs $24.99 at the Fora online store.
There aren't many user reviews of the Fora 6 Connect on major retailer sites, so your main option for viewing user feedback is via the Fora online shop. At the bottom you'll find a list of testimonials from Fora 6 Connect users, with most honing in on how easy the device is to use, how fast it is at producing results, and how it can check ketones and blood glucose readings. Fora Sterile Lancets and Testing Strips all have high user reviews on Amazon.
As a Bluetooth-enabled device, the Fora 6 Connect glucose meter saves readings to a companion phone app, iFORA HM (iOS, Android), so that you can dig into the data and pinpoint trends. Keeping readings is a vital part of diabetes management, especially if you are taking medication and want to see how effective it is. With the capacity to store 1,000 readings, the Fora 6 is a real ally here.
When used to test blood glucose, ForaCare’s six-parameter glucometer requires a small sample size (0.5 μL) to measure not just blood sugar, but also hematocrit concentration (HCT), hemoglobin (HB), β-Ketone (KB), Uric Acid (UA), and Total Cholesterol (TCH). This is valuable for advanced diabetes management, with results displayed in just five seconds.
The large display also makes this one of the best glucose meters for people with sight issues, as the numbers are easy to read, and the backlit display is comfortable to look at, especially in dimly-lit rooms. We’d advise reading through the Fora 6 Connect’s user manual to acquaint yourself with the various symbols shown on the display during a reading. To aid ease and accuracy of testing, the Fora 6 Connect is designed with a bright port light and an eject button.
While the Fora 6 Connect supports Alternative Site Testing (AST), so obtaining a blood sample from your palm, forearm or upper arm, AST is not suitable for everyone and should only be performed at certain times. We'd recommend speaking with your doctor first to see if this is suitable for you.
- Read our Fora 6 Connect review
Best glucose meter for small blood samples

Analyzing data from past blood sugar readings could help you spot potential trends, and Dario is one of the best glucose meters for doing just that. The no-coding Dario LC Blood Glucose Monitoring System works with a companion app (iOS 12+, Android) and automatically records results in-app, saving you the hassle of inputting data.
The Dario LC Blood Glucose System has over 2,900 reviews on Amazon, with an average rating of 4.3 out of 5 stars, while the product’s listing on Best Buy has 19 reviews, also scoring an average of 4.3 out of 5. The majority of reviews are positive, praising the meter’s compact size, ease of use, and large display. The minority of critical reviews focus on accuracy of results after a few weeks of use, though Dario says that 95% of measurements are within ±15% of the medical laboratory values.
The Dario LC Blood Glucose Monitoring System is also designed to provide analysis of your readings, and you can opt to share data with your doctor or healthcare professional as needed.
This glucometer is small and lightweight, which is essential if you’re carrying it with you throughout the day. You don’t have to fiddle around with batteries or charging cables either, as it connects directly to your phone via its charging port. The device tracks a variety of metrics including carb intake, exercise and medication.
Dario says that the meter can provide accurate readings in six seconds, and that ‘95% of Dario measurements are within ±15% of the medical laboratory values.’ There’s also an integrated hypoglycemia alert that can be used in tandem with your GPS location to help you stay safer. When you buy the starter kit, you’ll get the Dario glucose meter itself, plus 24 test strips, ten lancets and ten disposable covers.
- Read our Dario LC Blood Glucose System review
Best glucose meter for fast results (non-CGM)
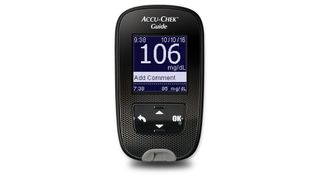
The Bluetooth-enabled Accu-Chek Guide Glucometer from Roche Diabetes is designed to be very simple to use for beginners upwards, with a clear display showing reading results in four seconds. According to the company, ‘95% of measured glucose results shall fall within ±10 mg/dL of lab reference value for blood glucose concentrations <100 mg/dL and within 10% for blood glucose concentrations ≥100 mg/dL.’
There are around 370 Accu-Chek Guide reviews on Amazon, averaging 4.6 out of 5 stars, with 89% of those being 4 stars and above. Positive user reviews focus around how simple the glucometer is to use, and how it is ‘almost’ pain-free, thanks to the included FastClix lancing device. Some critical reviews mention issues with pairing the meter, while others said early packaging was misleading, as it suggested strips were included when they have to be purchased separately.
Download the free Accu-Chek Connect App and sync the glucose meter, and it will automatically record your blood sugar readings to the app for you to analyze on demand. The backlight screen is bright and backed up by a port light that automatically comes on when you insert a test strip. This is handy if you have low vision, or if you are using the Accu-Chek Guide Glucometer in a darkened room.
There’s also a test strip eject button on the right-hand side of the glucose meter to aid usability and accuracy. And because the compatible test strips are quite light and small, this simple eject function is necessary so that you don’t have to fumble around. The anti-spill test strip storage pack is a nice touch - no more spilling strips when you take one out.
Roche has designed the test strips with ease of use in mind too, as you can add a small drop of blood for testing anywhere along the strip, as opposed to just in a specific spot. The suggested retail price for a 50-strip vial is around $30, or $49.99 for 100. There are subscription options too.
- Read our Accu-Check Guide review
Best glucose meter for fewer fingerprick tests

The Abbott FreeStyle Libre provides ‘flash glucose monitoring’ and reduces your need to take multiple fingerprick tests each day. Instead, this glucose meter works with a disposable 14-day sensor that’s applied to your upper arm, and a companion app (iOS, Android). As a system, the FreeStyle Libre tracks your glucose data for 90 days and provides instant readings whenever the sensor is scanned by the reader. The sensor’s blood glucose reading range is 40 to 500 mg/dL.
The FreeStyle Libre site features user ‘stories’ rather than reviews, and you can filter these by age range to read testimonials from people of a similar age. The majority of existing customers welcome the freedom and comfort of not having to do so many fingerprick tests, and praise how well the system works with the app. On the ProTherapySupplies store, a 5-star user review said, ‘Really love this and not needing to stick fingers!’
The Abbott FreeStyle Libre sensor measures the level of glucose in interstitial fluid, a method of measurement often used by continuous glucose monitors (CGMs). Still, experts recommend carrying out some standard blood glucose tests to ensure CGM-type devices are accurate.
As such, the reader works with FreeStyle Optium blood glucose test strips (the test strip port sits at the bottom of the reader). The reader measures 95 x 60 x 16mm and weighs 65g, and has a battery life of seven days typical use. The microUSB data port (for downloading readings) doubles as a charging port.
The amperometric electrochemical sensor, meanwhile, has an eight-hour memory, with glucose readings stored every 15 minutes. The sensor has a small, flexible tip that is inserted just beneath the skin. The reader will store up to 90 days’ worth of blood glucose data captured by the sensor, and you can enter notes regarding physical activity, food and insulin to help you better understand how they affect your blood glucose. Reports are generated in the companion app and can be shared with your doctor as needed.
To get a blood glucose reading, turn on the reader and hold it within 4cm (1.5 inches) of the sensor to scan it. The sensor then sends a wireless reading to the reader, with your current glucose level displayed on the reader’s touchscreen. You will see an arrow indicating whether your blood glucose is going up or down, but there is no hypo(glycaemia) alert here, which is a shame. If that's a deal-breaker for you, the One Touch Ultra 2 could be the best glucose meter for you.
- Read our Abbott FreeStyle Libre review
Best glucose meter for cheap test strips

If you’re new to testing your blood glucose levels, we’d recommend considering a complete kit that gives you everything you need to begin testing and to get used to what is involved. The Auvon DS-W Blood Sugar Kit is routinely flagged up as being simple to use, with high quality test strips designed to be more resistant to oxidation. However, as we have said throughout this guide, the best glucose meter for you is the one covered by your insurance.
There are over 80 user reviews on the Auvon website, but none of them state a specific date and instead just say ‘a year ago’. Together they generate a user review score of 4.1 out of 5 stars, with 66 awarding 4-stars and above. Some focus on affordability and ease of use, as well as accuracy, but some critical reviews questioned the accuracy, and how the meter requires a larger blood sample than some others. On Amazon there are over 1,470 reviews with an average rating of 4.6 out of 5 stars.
The Auvon DS-W Blood Sugar Kit uses test strips made using an automatic carbon printing technique to reduce interference and boost accuracy, and there is no coding required. If buying direct from Auvon, 50 test strips costs $8.99, or $21.99 for 150.
Auvon isn't clear about the blood sample size needed, which isn’t helpful, but plenty of user reviews mention that the lancing device isn’t as painful as others they have used. Auvon says this is because the lancet design should, ‘minimize vibrations and oscillations of the lancet needle, lessening the wound during collecting the blood, thus reducing the sense of pain.’
Auvon also claims high accuracy with its DS-W glucose meter, and that it functions within ±10%, or ±10 mg/dl of laboratory values 95% of the time. This handheld blood glucose monitor features a large digital display, with readings displayed in mg/dl. It will store continuous 7-, 14- and 30-day average results to give you greater insight. The Auvon DS-W Blood Sugar Kit features in a number of prominent glucometer roundups, and has largely positive user reviews, so could be worth discussing with your diabetes healthcare provider.
Best glucose meter for spoken results

The Prodigy Voice is designed for blood glucose testing using fresh capillary whole blood samples, and is the only glucometer to receive an Access Award from the American Foundation for the Blind (AFB) and an Access Plus Award from the National Federation of the Blind (NFB). As it reads results aloud, it’s considered the best glucose meter for people with no or low vision. It’s also a good choice for people with dyslexia or who encounter discomfort when reading digital screens.
There are over 700 user reviews of the Prodigy Voice Glucose Meter on Amazon, with an average rating of 4.5 out of 5 stars. 88% of them are 4-star rated and above. As with every glucose monitor in this guide, while the majority of people praise the accuracy, a minority are critical of it.
When the audio function is activated, the Prodigy Voice will welcome you and state the day and time, then it will tell you to apply your blood sample to the test strip. After six seconds it will then read aloud your blood glucose (number) milligrams per deciliter/millimoles per liter.
There’s a button you can press to repeat the last spoken result, just in case you missed what was said, and there are imprinted buttons with tactile markings, including directional arrows and letters, to enable blind users to easily find and use them. On the side you’ll find volume controls and a headphone port for private listening to spoken results.
The Prodigy Voice Glucose Meter stores 450 audible test results, and dishes out 7-, 14-, 21-, 30-, 60- and 90-day averages, so there’s plenty of data on offer here. And via the USB port you can connect the glucometer to your computer to download readings using the included, free diabetes management software. This is ideal if you want to share readings with your doctor.
In the box you’ll get the Prodigy Voice Meter, control solution, a lancing device, 10 sterile lancets, 10 Prodigy Blood Glucose Strips, and two 1.5 V AAA alkaline batteries, all packaged in a carry case. While you can use it for Alternative Site Testing, we’d recommend speaking to your doctor about whether this is right for you, and when you should and shouldn’t use AST.
- Read our Prodigy Voice review
The best glucose meter for ease of use

The Contour Next EZ Glucose Meter is primarily aimed at beginners or those who don’t want a lot of fuss of high-end features when testing their blood sugar levels at home.
As such, it’s very simple in its design and what it offers, and while this isn’t necessarily a bad thing, it does mean that you should look elsewhere in our best glucose meters guide if you want smart connectivity or sensors.
The Next EZ Glucose Meter requires you a small blood sample in order to read your blood glucose levels, and returns results within five seconds. A lancing device and replaceable lancets are included with this blood sugar monitor kit, as well as test strips, though you will soon need to buy new strips.
There are over 140 user reviews of the Contour EZ Glucose Meter on Walmart, with an average rating of 4.5 out of 5 stars. 106 of those of 5-star reviews. So the majority of customers are highly praising, though a few reported not having any test strips in the box.
The cost of these ranges depending on where you shop, but Contour offers a loyalty scheme that could give you access to bigger savings when buying direct. Speak to your insurance provider to see what they will cover.
What we also like about the Contour Next EZ Glucose Meter is the large, easy to read display, and how it’s very self-explanatory straight out of the box. This is one of the best glucometers for covering the basics of blood sugar testing at home, and stores up to 480 readings at a time. Don’t forget that you can download this to look over, which could help you to spot potential trends behind your blood glucose levels.
- Read our Contour Next EZ Meter review
Best glucose meter for seniors

The Care Touch glucometer is relatively inexpensive compared to others, and that’s because it opts for a basic design with little in the way of fancy frills. But that means it’s also simple to use, and is ideal for seniors experiencing sight issues as the display is large, uncluttered, and uses big numbers for at-a-glance readings.
Speaking of fast, the Care Touch Blood Glucose Monitoring System delivers a result in five seconds, which is on par with some of the more premium blood sugar monitors.
As an older model, it’s no surprise to see that the Care Touch glucometer has over 13,000 user reviews on Amazon, generating an average score of 4.6 out of 5 stars. 90% of those reviews are rated 4 stars and above, and focus on the affordability, ease of use, the large and simple display, and how accurate it is for a cheaper meter. Users also praise how compact the meter is. Critical reviews focus on customer service, battery life, and some accuracy concerns, which are echoed in a Walmart user review.
Although it’s a cheap glucometer, you can still annotate the readings with information such as ‘pre-meal’ or ‘post-exercise’. Your doctor may recommend that you keep consistent notes when taking readings so that you have extra insight into potential causes for spikes and crashes.
The Care Touch Blood Glucose Monitoring System can be purchased as a complete kit, including the meter itself, plus 100 test strips, a lancing device, 30 disposable lancets, and a battery. A carry bag keeps it all together, though it’s quite bulky.
In addition to recommending this glucose meter for seniors, it could be helpful to beginners who don’t want to spend a great deal on blood sugar monitoring until they are comfortable with it.
The Care Touch Blood Glucose Monitoring System is also well-suited to people who feel swamped by too much data, and would prefer something basic yet accurate. On that note, there is no companion app for the Care Touch glucometer, but it does hold 300 readings that you can download to your computer to look through and spot trends.
It also produces a 14-day average, though if you want longer averages, also consider the One Touch Ultra 2 or the Auvon Glucose Meter. Other benefits with the Touch Blood Glucose Monitoring System include no coding, and an eject button to easily dispose of used test strips.
While we are disappointed by the lack of a port light to boost visibility when inserting new test strips, it’s important to note that this is quite an old model now compared to newer glucometers. So if you want the latest diabetes tech, look elsewhere. If not, for the low price this is worth considering.
Best glucose meter for basic testing

The One Touch Ultra 2 Blood Glucose Meter is a popular blood sugar monitor, designed to store 7-, 14- and 30-day average results. It works with OneTouch Ultra test strips that use DoubleSure technology to automatically check your blood sample twice to boost accuracy.
As with other top glucose meters, you can use a control solution to check that your One Touch meter and test strips are working properly.
At Amazon, the One Touch Ultra 2 has over 1,200 user reviews, generating an average of 4.4 out of 5 stars. 85% of those are rated 4 stars and above, and focus mainly on the meter’s ease of use and accuracy. Many recommend it for beginners, though some question the price of test strips. Critical reviews say meter they received became less accurate with time, and that it ran high compared to other meters. At Walmart, 40+ user reviews generated a lower average of 3.5 out of 5 stars, with some praising its ease of use, while others said the display was dim.
The One Touch Ultra 2 is cleared for Alternative Site Testing, such as from your palm instead of your finger - always follow guidelines as to when to use AST and when to avoid it. Each time you use the meter to take a blood sugar reading, you can label them pre- or post-meal to help you see, at a glance, how food affects your blood glucose. You can also add notes about exercise, stress and medication.
The One Touch Ultra 2 comes with two lithium batteries (3.0 volt CR 2032), so you can use it straight out of the box. Also included is a OneTouch Delica Plus lancing device, equipped with 13 depth settings for more precise lancing. The Delica Plus comes with 30-gauge and 33-gauge (extra fine) heads - 10 sterile lancet heads are included, with everything packaged into a carry case.
The large digital screen is backlit to aid readability, with the results clearly displayed. As mentioned above, the One Touch Ultra 2 stores up to 500 readings, and measures in mg/dl. You will have to code your new test strip vial before using them with the meter, which could put some people off.
Importantly, the glucose meter has low glucose and high glucose alerts, and what you should do in each instance. Again, we’d recommend reading the user manual to ensure this glucometer will do what you need it to, ahead of purchasing.
- Read our One Touch Ultra 2 review
Best glucose meter for built-in alarms

This self monitoring blood glucose meter requires no coding, making it one of the easiest blood sugar monitors for beginners. Like the other devices featured in our best glucometers roundup, it produces fast results with minimal fuss.
The Trividia Health True Metrix Blood Glucose Meter stores approximately 500 readings, and these can be downloaded onto your computer for storage.
This meter has over 190 reviews on Amazon, scoring an average of 4.6 out of 5 stars. 89% of those are rated highly, and highlight the meter’s accuracy and reliability. Value for money is another common motif. Again, like all the other glucometers in this guide, a minority of reviews criticize the accuracy and battery life. From 350 reviews on Walgreens, the meter scores a lower 3.6 out of 5, with 209 being 5-star reviews, and 71 being 1-star reviews. Critical reviews state that the meter is inconsistent, while positive reviews say it has never faltered in its accuracy.
The meter offers 7-, 14-, 30-, 60- and 90-day averages to help you determine if your diabetes management routine or medication are working or need to be adjusted with your doctor’s guidance.
You can tag blood sugar results by linking them to specific instances such as pre- or post-meal, when taking medicine, or after exercising. The True Metrix Blood Glucose Meter has four programmable alarms to remind you to test your blood sugar levels – handy if you often forget to do so – and it has a ketone reminder.
As for the design, the glucometer has a test strip release button to help you avoid touching the strip after testing. The 0.5 microlitre sample means it should feel less painful to draw blood from your fingertip or the side of your fingers.
You could also try Alternative Site Testing with this glucometer, as long as your doctor is in favor and explains when it should and shouldn’t be used.
- Read our True Metrix review
Best glucose meters: The Final Word
Why you can trust Top Ten Reviews
Glucose meters wear out over time and should be renewed every two years to ensure accurate and reliable results. Before buying a glucose meter, check with your insurance provider to see what they will cover. That includes test strips compatible with the glucometer you’re thinking of purchasing, as strips can drive up the overall cost in the long-term.
Once you know where you stand with your insurer, you can then make a shortlist of the best glucose meters within your budget range. Look for features that will make your life easier, such as a large display, or data storage for multiple readings. Keep the size in mind too, as you’ll be carrying your blood sugar testing kit with you throughout the day.
Ultimately, a glucose meter is only good for you if it works for your diagnosis, your lifestyle and your budget. If you’re really stuck and still don’t know which glucometer to choose, ask your doctor or a diabetes health expert if they can make some recommendations – even a steer on brands will point you in the right direction.
The latest prices on the best glucose meters
What are the best glucose meter brands?
When you begin researching glucometers, you’ll see certain brand names pop up time and again. Some brands, including One Drop, are relatively new, while others have been established in the blood sugar monitor market for a long time.
These are some (but not all) of the brands you’re likely to come across during your research, listed in alphabetical order:
- Abbot Diabetes Care
- Advocate
- Agamatrix
- Arcadia Group
- Arkray
- Ascensia Diabetes Care
- CVS
- Dario Health
- Dexcom
- Diathrive
- Foracare
- Genesis Health Technologies
- iHealth
- One Drop
- Prodigy Diabetes Care
- Roche
- Trividia Health
- Walmart
Best glucose meters: The different types
Currently, there are three main types of glucose meter:
- Basic blood glucose meters
- Continuous glucose monitors (CGMs)
- CGM-Insulin Pump Combos
The most simple glucometers are handheld devices with a digital screen that displays a reading, and these are the devices we’re mostly focusing on with our guide to the best glucose meters. These readings are gathered from disposable blood sugar test strips treated with specific chemicals that react to glucose. A new test strip is inserted into the glucometer for each new reading.
Standard glucometers are usually battery operated and capable of storing readings, and many can be connected to a computer so that you can download and store your readings to look back on as needed.
Some basic blood glucose meters are designed with a spring-loaded needle (the lancing device) that pricks the side of your fingertip to draw a small drop of blood for testing. Others use an external lancing device.

Once blood is drawn, you touch it to the test strip, which will absorb your blood sample and display a reading on the glucometer’s screen. While response times vary between blood sugar monitors, we’re usually talking seconds.
Some glucose meters are approved for Alternate Site Testing (AST). That means they give results within 20% of correct values when used on alternative sites such as the palm, forearm or thigh. However, Diabetes Self Management advises that, ‘you should still check alternate site readings on yourself before trusting them too much.’
Diabetes UK says that, ‘According to reports, routine blood glucose level testing before meals or two or more hours after meals from alternate sites are equivalent to fingertip testing. However, glucose arrives faster in the fingertips than in the arms. Therefore, testing when blood glucose is falling rapidly or rising rapidly is likely to be less accurate from alternate sites.'
Continuous glucose monitoring vs standard
Continuous glucose monitors use a sensor that is placed under your skin, where it measures your blood sugar levels and sends frequent readings to a recording device worn on your person. Some CGMs can be programmed to sound an alert if it senses your blood glucose levels are too low or high.
When we spoke to diabetes educator and nurse clinician Susan Stauffer, BSN, RN, CDE, she explained how, “A Continuous Glucose Monitor has a sensor that must be inserted into subcutaneous tissue with a needle that then leaves the small sensor below the skin. CGM devices are wonderful alternatives to routine blood glucose testing, however, not all people need these devices and they are expensive to use.
“The accuracy of both the Dexcom G6 and the Freestyle Libre have proven to be as good if not better than blood glucose meters,” continues Stauffer, “and the FDA has approved the BG number to be used for insulin dosing.”
There are four FDA-approved CGMs available to buy, and they are made by Abbot, Dexcom, Senseonics, and Medtronic. These devices are more expensive than basic glucose meters and vary from around $300 to several hundred.
The replaceable sensors, most of which need to be changed every one to two weeks, cost $40-$60 each. You might also need to use a standard glucose meter to confirm the blood sugar level readings and to program the CGM – never use results from an alternative sampling site to calibrate a CGM.
Research shows that 24/7 glucose monitoring helps lower the risk of hypoglycemia and hyperglycemia, and CGMs can be beneficial to some people with Type 1 and Type 2 diabetes who struggle with maintaining their target blood sugar. CGMs can also help you pinpoint lows even if you’re unsure they’re happening (hypoglycemia unawareness).
Best glucose meters buying advice
How to choose the best glucose meter for you
When picking a good glucose meter, there are specific features that can make your life easier when taking regular blood sugar readings at home. According to the Mayo Clinic, accuracy should quite rightly be top of the list. ‘Some meters are known for giving readings that show blood glucose levels up to 15% higher or lower than they actually are. That variance is accepted by the Food and Drug Administration, but the more accurate readings you can get from your glucometer, the better.’
Other features to look for when choosing the best glucose meter for you include:
Insurance – When you’re testing your blood glucose multiple times a day, the cost of test strips ramps up, so speak to your insurance provider to see what they’re prepared to cover, whether that’s the full cost or a portion of it.
Ease of use – Most diabetics use a glucose meter throughout the day, so choose one that is simple to use and has a lancing device size that feels more comfortable to you.
Display – Large displays make it easier for you to see and read your test results quickly. Bluetooth-connected smart glucometers take this a step further by storing your readings in an app that you can view on your phone.
Spoken results – If you have low vision, the best glucose meter for you is the one that speaks your blood sugar reading test results aloud.
Data storage – The average glucose meter can store upwards of 50 readings, but smart glucometers can store ten times that. The more readings you have access to, the easier it will be for you and your doctor to pinpoint trends over time. Again, check with your insurer first to see if they’ll cover such a device.
Blood sample size – Different glucose meters require different sizes of blood droplets on compatible test strips. Diabetes.org has produced an excellent guide to blood sample sizes required by mainstream glucose meters for personal use.
Kristen Scheney, a nutritionist for CCS Medical, recommends not using price as an indication of quality. She says, "just because one glucometer is more expensive than another does not mean that it will be more accurate.
"Moreover, just because a device includes more features than another does not mean that it is the device for you. Sometimes simple is the best way to go to ensure you’re getting exactly what you need out of your glucometer."
Best glucose meters FAQ
How do you use a glucose meter?
Always read the full instructions for a glucometer before using it, and note down any specific instructions given to you about glucose meter use by your doctor. The basic approach when using a blood sugar monitor is to wash your hands thoroughly, then insert a new disposable test strip into the meter.
Next, prick your finger with a lancet to draw a drop of blood. Now carefully place that finger against the test strip (in the correct spot, if stated), which has been treated with chemicals to enable it to react with glucose. In America, glucose meters report test results in milligrams of glucose per deciliter of blood (mg/dl).

When should I replace my glucose meter?
This depends on the glucometer you buy, but Diabetes Forecast says that, "It may be time to replace or upgrade your meter to a newer model if it’s older than five years and you can get one with a lower monthly cost, increased accuracy, and with features such as a smartphone app."
Generally speaking, modern glucose meters have better functionality, provide faster readings, and don’t require coding when you open a new vial of test strips. This will make your life easier, and ensure that whichever of the best glucose meters you choose, it fits around your lifestyle.
When should I test my blood sugar with a glucometer?
Always follow your doctor's recommendations about how often you should test your glucose, as you may need to test your blood sugar levels several times a day to make necessary adjustments to your diet, activity or medication.
According to the CDC’s blood sugar management advice, ‘how often you check your blood sugar depends on the type of diabetes you have and if you take any diabetes medicines’. Your doctor may also want to check your blood sugar more frequently if you take insulin. Common times to test your blood sugar include:
- When you wake up, before eating or drinking
- Before you eat a meal
- Two hours after eating a meal
- When you go to bed

How accurate are the best glucose meters?
You’d be forgiven for thinking that all glucometers have FDA clearance because they are medical devices, but that isn’t always so. The 2018 FDA draft guidance for personal use glucose meters will require:
- 95% within +/- 15% across the measuring range
- 99% within +/- 20% across the measuring range
Research conducted by The Diabetes Technology Society Blood Glucose System Surveillance Program found that accuracy varied widely between the major home blood glucose meters. At present, they are considered clinically accurate if the reading is within 20% of what a lab test would indicate. The quality of the glucometer and compatible testing strips can impact the overall accuracy of your blood sugar monitoring test.
How accurate your glucometer is depends on the quality of the device itself and the quality of compatible test strips. We’d also recommend checking the instructions for the meter to see what substances (eg, vitamin C) might interfere with blood sugar reading accuracy.
Finally, store the glucose meter and test strips according to the manufacturers’ instructions, as incorrect storage may also impact accuracy of readings. Test strip vials, for example, should be closed when stored. This is backed by research, published by the National Library of Medicine, that showed how ‘test strip stability lasted longer for closed vials than open vials.
For open vials in adverse storage conditions, the refrigerator environment offered the longest stability at 35 to 50 days, and direct light and humidity offered the shortest periods of stability at 3 to 14 days.’
Are glucometers hygienic?
When using a glucose meter, always follow the instructions set out by the manufacturer or as advised by your doctor. As basic blood sugar monitors require a blood sample for testing, it’s vital to practice hygiene and lancing hygiene when using the device.
On this note, the CDC recommends the following:
- Whenever possible, blood glucose meters should be assigned to an individual person and not be shared.
- If blood glucose meters have to be shared, clean and disinfect it after every use, per manufacturer’s instructions, to prevent carry-over of blood and infectious agents. If the manufacturer offers no guidance on how the meter should be cleaned and disinfected, do not share the device.

What is hypoglycemia?
When your blood sugar is low, you experience hypoglycemia. Diabetics are at a high risk for hypoglycemia because of the medications they take to keep their glucose levels down. Since your body either doesn’t produce insulin or doesn’t produce enough insulin, you have to be careful to not let your glucose levels get too high.
This means you either take medications or limiting the carbohydrates in your diet. Diabetes is largely a balancing act of trying to keep your glucose from going too high while also making sure it doesn’t get too low.
Here are some of the common symptoms of hypoglycemia:
- An irregular heart rhythm
- Fatigue
- Pale skin
- Dry mouth and throat
- Shakiness
- Anxiety
- Sweating
- Hunger
- Irritability
- Tingling sensation around the mouth
- Crying out during sleep
Severe hypoglycemia results in confusion, abnormal behavior, visual disturbances, seizures and, ultimately, unconsciousness.
Glucose meters glossary
Adult-onset diabetes – an old term for Type 2 diabetes.
Calorie – a unit of energy that comes from food.
Carbohydrate – according to WebMD, carbohydrates are one of the three main classes of foods and an energy source. Carbs mainly consist of sugars and starches that the body breaks down into glucose.
Certified diabetes educator (CDE) – a health professional certified by the National Certification Board for Diabetes Educators to help people with diabetes learn how to manage and live with their condition.
Continuous Glucose Monitor (CGM) – a sensor and wearable reader duo that takes very regular glucose level readings.
Dietitian – a registered expert able to help people understand what types of foods to eat and avoid for optimal health.
Glucagon – Medicine.Net describes a glucagon is a hormone that causes the liver to release glucose into the blood.
Glucose – a simple sugar found in blood. It’s the body’s major source of energy
Glucose tolerance test – according to a Patient.Info explainer, a glucose tolerance test identifies how well (or not) your body handles glucose after a meal.
Hyperglycemia – high blood sugar.
Hypoglycemia – low blood glucose.
Injection site – clinically recommended places on the body to inject insulin, such as the abdomen and thighs.
Insulin – a hormone produced in the pancreas to regulate the amount of glucose in the blood.
Lancet – a fine needle for pricking the skin during blood sugar testing.
Mg/dl (milligrams per deciliter) – a measurement indicating how much glucose is in a specific amount of blood.
Self monitoring of blood glucose – measuring how much sugar is in your blood
Type 1 diabetes – the CDC says Type 1 diabetes is a condition where ‘your pancreas doesn’t make insulin or makes very little insulin. Insulin helps blood sugar enter cells where it can be used for energy. Without insulin, blood sugar can’t get into cells and builds up in the bloodstream.’
Type 2 diabetes – according to advice published by Diabetes.Org, Type 2 diabetes is when your body doesn't use insulin properly.’ As a result, glucose cannot get into the body’s cells for use as energy.
Resources for people with diabetes
Diabetes.org: The American Diabetes Association is the online authority on diabetes. If you or a loved one have diabetes, becoming a member is a great idea. The association is devoted to education, prevention, community and meal planning.
Diabetes Forecast: A partner of The Healthy Living Magazine, this resource includes consumer guides on diabetes products and medicines, as well as recipes and tips for taking care of the psychological impacts of living with diabetes.
diaTribe: Excellent resource for finding the latest academic studies on diabetes and clinical trials currently underway, including how you might be able to take part in the trials.
DiabeticGourmet: A website and magazine of diabetic-friendly recipes, diet tips and resources. You can register for free and keep track of your favorite recipes, connect with others on a forum, and receive tips for better management.
Diabetes Food Hub: A partner of the American Diabetes Association, this website is devoted to providing diabetic-friendly recipes and meal planning.
Beyond Type 1: A community of over 2 million people in over 150 countries. This website features programs, stories and news on Type 1 diabetes.
John Hopkins Patient Guide to Diabetes: One of the most comprehensive online resources for diabetes articles, news, terminology, treatments and tools.
Six Until Me: A popular blog-style website created by Kerri Morrone Sparling where she shares inspiring essays and stories about her life with diabetes. She includes interviews with experts and advocates for products and diets that work for her.
Diabetes Monitor: A comprehensive collection of articles and information related to Type 1 and Type 2 diabetes. The site connects you to experts and to a community called the Diabetes Collective.
Diabetes Exercise News & Organization: A resource for exercise-related articles to help with home-monitoring, recognizing symptoms and managing complications.
Diabetes Daily: A daily home for news, tips, articles, guides and stories about people living with diabetes.
Diabetes Training Camp: A non-profit foundation devoted to week-long and weekend camps designed to inspire, motivate, and educate people with diabetes so they can thrive.
Further health and wellness guides

Moving your body is important for overall health, and walking is a good place to start. With a treadmill, you can do it indoors.



