Best air purifiers: top picks to breathe cleaner year-round, tried and tested
The best air purifiers, often packing HEPA filters, will clean your air of allergens, dust and more.

Sign up to receive the latest news, reviews, buying guides and deals direct to your inbox
You are now subscribed
Your newsletter sign-up was successful
Finding the best air purifiers can help make your home cleaner, meaning fewer allergens and potentially harmful pollutants. This isn't just for those with allergies or young children, but anyone who wants to lower the toxic load in their system by breathing purer air. Expect to find HEPA filters in many models, as these are the go-to choice for efficient particulate absorption.
Air filters can trap dust and pet dander, which can potentially cause allergic reactions in homes. But they're not the only feature to look out for when finding the best air purifiers. Keep an eye on the CADR or Clean Air Delivery Rate, as this is the number that signifies how fast the model will be able to clean your property's air. Have large rooms? Go for a higher CADR number.
You may want to think about other features, which can vary the price but add elements of premium luxury to the result. For example, some purifiers can add essential oils, allowing you to create a lovely scent in your home to accompany that cleaner air. Or, if you want this for sleeping, you may think about a quieter and more energy-efficient model that can run in your bedroom overnight. Around 52 decibels, at full power, is what you'll want or lower ideally.
You may also want to consider the best dehumidifiers to fight condensation and mold. If you struggle with dry air, the best humidifiers could help. Or read on to find the best air purifiers out there right now.
The best air purifiers we recommend
Why you can trust Top Ten Reviews
The best air purifier overall

Specifications
Reasons to buy
Reasons to avoid
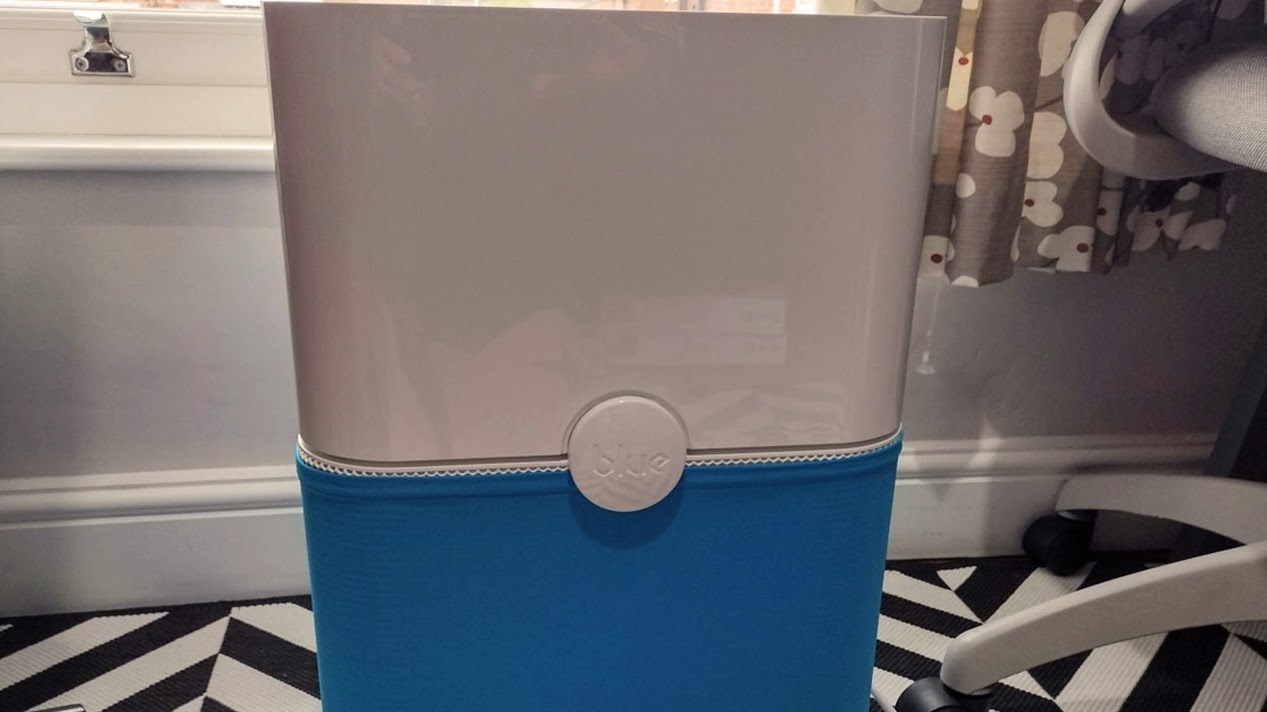
🔎 The Blue Pure 211+ air purifier is a reliable and powerful device with a simple design and energy efficiency. Although it lacks smart features, it offers excellent performance results. Although it may be pricey and bulky, it's a great value for money. ★★★★½
If you're looking for a reliable and powerful air purifier that can effectively clean the air in a large room, the Blue Pure 211+ may be the answer.
Design: The Blue Pure 211+ is a sturdy and heavy air purifier that may not be the easiest to move around. However, it has an attractive stencil cut-out at the top and customizable fabric sleeves that match your home décor. If you remove the fabric sleeve, you'll find a mesh base that looks clean and stylish but may accumulate dust over time.
Performance: We conducted a series of tests on the Blue Pure 211+ air purifier in a sealed room measuring 323 square feet. Our tests were conducted over three 30-minute trials using an air particle counter before, during, and after testing. We evaluated the cleaner's ability to tackle ambient air quality, its effectiveness in handling incense smoke, and its ability to absorb particles released by burning matches.
The results were impressive, with the Blue Pure 211+ absorbing 93% of particles smaller than 0.3 microns and 88% smaller than 2.5 microns at the lowest setting and 99.9% smaller than 0.3 microns and 100% smaller than 2.5 microns at its highest setting. It also absorbed 100% of particles measuring smaller than 10 microns. The Blue Pure 211+ outperformed most other air purifiers, including the much more expensive Dyson Purifier Cool, making it one of the most powerful and effective air purifiers we tested.
Value: The Blue Pure 211+ is a top-performing air purifier that can be purchased from BlueAir.com, Home Depot, or Amazon. While it's pricier than other options, it offers excellent value for its large square footage capability. The Levoit Core 400S is a more affordable alternative, while the Dyson Purifier Cool adds style and wow factor. If you're on a budget and have limited space, the KOIOS EP1810 is a great option.
Read more: Blueair Blue Pure 211+ review
The best air purifier on a budget



Specifications
Reasons to buy
Reasons to avoid
🔎 The Levoit H132 is an affordable and compact air purifier that works well in small rooms but is not suitable for larger ones. It runs quietly and could be a good option for those on a budget. ★★★½
The Levoit air purifier is affordable, compact, and runs quietly, making it suitable for small rooms. However, its performance was disappointing during testing, particularly for smaller particles. It's a good budget option with a 2-year warranty and a 30-day money-back guarantee.
Design: The Levoit air purifier is a decent-looking device, but it lacks the sophistication of other models in the same price range. Its shiny plastic finish is less elegant than the Levoit 400S or the Koios air purifier, which is half the price. However, its neutral color and compact size make it easy to blend into any room. The most striking features are the grooved indentations on the base and the fan wheel at the top. If you don't want your air purifier to be a talking point, it can be easily stowed on a shelf or side table.
Performance: We tested the Levoit H132 air purifier and were impressed with its features, such as the dimmable night light and the handy memory function. However, during our tests, we were disappointed with its overall performance. We conducted three different trials to evaluate its effectiveness: a match test, an incense test, and an ambient air quality test. During the ambient air quality test, the Levoit H132 struggled to absorb particles smaller than 2.5 microns, managing only 76%, while it absorbed 100% of larger particles measuring 10 microns.
The match test showed it absorbed only 68% of particles smaller than 0.3 microns and 69% smaller than 2.5 microns. However, the incense smoke test had much better results, with the Levoit H132 absorbing an impressive 96% of particles smaller than 0.3 microns, 87% smaller than 2.5 microns, and 98% smaller than 10 microns.
Value: The Levoit H132 is an affordable air purifier with free shipping, a 2-year warranty, and a 30-day money-back guarantee. For a smaller option, consider the KOIOS EPI810. For a higher performance, the Levoit 400S is a better choice. For a stylish option, check out the Dyson Purifier Cool.
Read more: Levoit H132 review
The best air purifier for nursery


Specifications
Reasons to buy
Reasons to avoid
🔎 The Levoit Core 400S is an affordable air purifier with top-end features and performance, making it a great choice. It has a sleek design and smart features and is cheap enough to buy multiple units. However, the VeSync app used to control it may be unreliable for some users. ★★★★½
The Levoit Core 400S is a sleek, affordable air purifier that outperforms more expensive models. Its smart features and top-end performance make it a great choice, but some users may experience issues with the VeSync app.
Design: The Levoit 400S air purifier is a sleek, white cylinder that weighs only 11 pounds and is easy to move around with two handles on either side. Its black vented wheel at the top holds a display screen that shows air quality data, fan settings, filter status, auto mode, and sleep mode. You can lock the display to show data all the time or set it to off. The casing is made with a smooth and matte finish, giving the cleaner an expensive and sleek look.
Performance: The Levoit Core 400S air purifier claims to purify the air in minutes, and a series of home-based trials were conducted to test its performance. The tests included assessing its performance on ambient air quality, a match smoke test, and an incense smoke test. It was also compared in different settings to determine how well it performed.
During the ambient air quality test, the Levoit Core 400S absorbed an impressive 99.5% of particles smaller than 0.3 microns and 100% smaller than 2.5 microns and 10 microns. Even at the highest setting, the volume level of the cleaner does not rise above that of normal conversation. The Levoit Core 400S performed significantly better than expected during the match test, absorbing 99.8% of particles smaller than 0.3 microns. The final test examined how well the cleaner absorbed particles released from incense cones. At level 4, it absorbed almost 100% of particles smaller than 2.5 microns and 10 microns.
Value: The Levoit Core 400S is a mid-range air purifier with smart and connected technology. It outperforms more expensive models, such as the Dyson Purifier Cool. For a compact option, consider the Levoit H132, and for larger rooms, the Blue Pure 211+ is ideal.
Read more: Levoit Core 400S review
The best smart air purifier

Specifications
Reasons to buy
Reasons to avoid
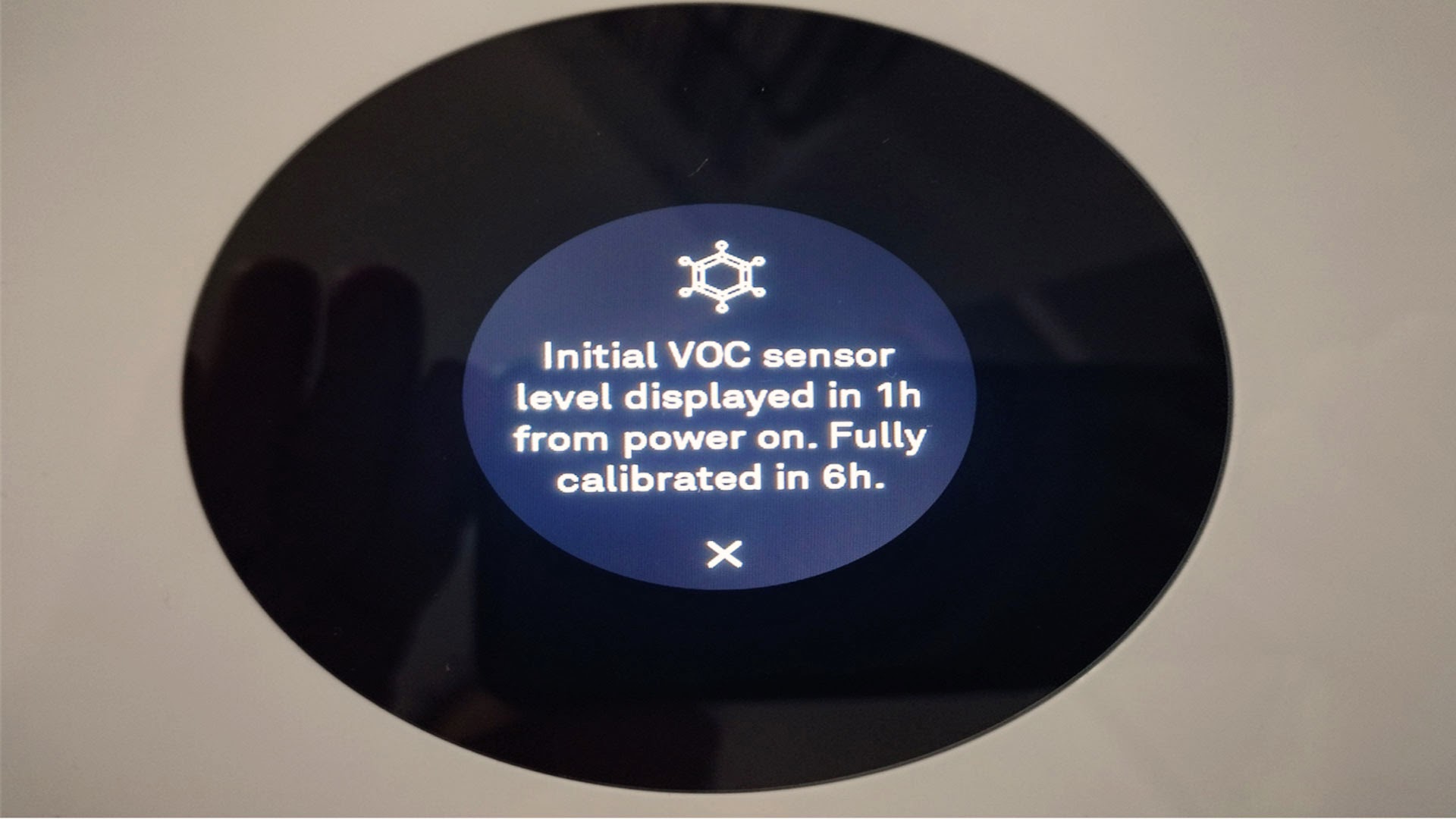
🔎 The Mila air purifier is packed with sensors and works with a great app, but it can be loud and has a large footprint. The replaceable filters are pricey, and there's no voice control. It's a great choice if you want data and specific health filters, but it may be too much for basic needs. ★★★★½
The Mila air purifier is a compact device that offers certified HEPA filtration and a Dual-Flow filter. It features eight air quality sensors, tracks carbon dioxide and monoxide, and works with various custom filters. It's a great choice for data and specific health filters, but it can be loud and has a large footprint.
Design: The Mila air purifier is stylish and compact, with touch controls to switch between auto and manual modes. It features certified HEPA filtration and a patent-pending Dual-Flow filter for enhanced odor and VOC filtration. Lab testing proves it can filter up to 95.7% of airborne viruses in 30 minutes. It delivers 447 CADR m3/hr of cleaning power, which is impressive.
Performance: The Mila air purifier is a versatile and innovative device with various features to improve indoor air quality. Its Automagic Settings include three sleep-friendly options: Sleep Mode, Turndown Service, and Whitenoise Mode. The Mila is designed to work with seven custom filters, each addressing health and wellness needs. While some cleaners have washable filters, the Mila uses high-tech filters that should be replaced every six months.
The device features eight air quality sensors that capture real-time data, measuring micro-particles as small as 0.01 microns wide through VOCs and humidity. The algorithm detects what is happening in the air and cleans it quickly. Additionally, the Mila tracks carbon dioxide and carbon monoxide and alerts users if it detects the latter, making it a handy device for improving indoor air quality.
Value: The Mila Air Purifier, which raised over $1.5 million on Kickstarter, is now available on the brand's website and Amazon. The product costs $349, with replaceable filters starting at $59. The Honeywell HPA300 Air Purifier is a cheaper alternative but not as powerful or feature-rich.
Read more: Mila Air Purifier review
The best air purifier for fan speeds



Specifications
Reasons to buy
Reasons to avoid
🔎 The Dyson Purifier Cool's impressive design and real-time data on air quality make it a hit with allergy sufferers. However, its high price tag and lack of fan power may make it unappealing for those on a budget or seeking a quieter home or office use option. ★★★★
The Dyson Purifier Cool is a stylish air purifier that cleans up to 800 sq. ft. and features ten power settings and auto and night modes. While it has a sleek design and real-time air quality data display, its high price and lack of fan power may make it unappealing for some users.
Design: The Dyson Purifier Cool is a sleek and stylish air purifier in two colorways: white/silver or black/nickel. It's a great conversation starter in any room, and its simple color scheme allows it to blend with most interior decor styles. The purifier is sturdy enough not to worry about pets or children knocking it over, but those with limited space may find it too large for their room. The contemporary, bladeless cooling loop perched above a silver perforated cylinder looks great from afar and up close, making it an attractive addition to any home.
Performance: The Dyson Air Purifier Cool is a powerful device that claims to clean up to 800 sq. ft. with its ten power settings, auto mode, and night mode. It also features a sleep timer to power off the device when you go to bed. However, during our tests, the purifier fell short of its manufacturer's claim that it could remove 99.95% of particles.
While it performed well in our first two trials, removing a significant percentage of particles at levels 6 and 10, it struggled in the third. To remove a high percentage of particles caused by burning matches, the purifier must be on its highest setting, making it quite noisy. As a result, it may not be suitable for some households or offices. Moreover, during our testing, a cheaper air purifier could remove more air particles at the same time.
Value: The Dyson Purifier Cool has a high price tag but has a 2-year warranty. Limited-time offers are available through the Dyson website or selected retailers. Consider the Levoit 400S for a similar performance at a lower price or the Blue Pure 211+ for large spaces. The KOIOS EPI810 is a compact option for desktops or travel.
Read more: Dyson Purifier Cool review
The best air purifier for large rooms


Specifications
Reasons to buy
Reasons to avoid
🔎 The Molekule Air Pro looks great and has a simple interface, but it doesn't effectively purify indoor air. Despite its high price and promotion, it didn't perform as well as a HEPA filter. For better value, consider another option from our range of tested purifiers. ★★★
The Molekule Air Pro is a stylish air purifier designed to cover large areas, but it didn't perform as well as other air purifiers in tests.
Design: The Molekule Air Pro is a stylish air purifier covering up to 1000 sq ft, making it ideal for large rooms and business premises. It weighs 22.9 lbs and features a vegan leather handle for easy movement. The device has a sleek cylinder design, silver casing, and touch-screen interface, giving it a premium, polished look. The neutral white base curves inward, resembling that of a lamp. The touch-screen display sits at the center of a 'wheel' at the top of the device, and when in standby mode, it features a simple glowing disc.
Performance: In our tests, we evaluated the performance of the Molekule Air Pro Professional air purifier in a 220 sq ft room. We tested ambient air quality before and after using the purifier, alongside incense and match smoke tests. The trials were conducted for 30 minutes to evaluate the purifier's ability to trap and remove air particles. We first ran the trials at the highest setting, level 3, below 50 decibels. Then, we re-ran the same trials at the highest level, 6, powerful but extremely noisy 71 decibels.
Based on these limited tests, we found that at its highest level, the Molekule Air Pro Professional did a fairly good job of removing larger particles in 30 minutes. However, its ability to improve ambient air quality was not as good as other air purifiers we tested at home. The purifier captured 67% of particles smaller than 0.3 microns and 64% smaller than 2.5 microns when running at level 3 fan speed. At the highest fan speed, the purifier removed 91% of particles smaller than 0.3 microns and 83% smaller than 2.5 microns. While it removed 98% of particles measuring 2.5 microns and 99% of particles measuring 10 microns during the incense test, it failed to meet expectations for its price point.
Value: For a stylish air purifier that performs well, consider the Dyson Purifier Cool. The Levoit 400S is a sleek and affordable option. If you need a compact purifier, the KOIOS EPI810 packs a True HEPA filter and weighs only 2.5 lbs.
Read more: Molekule Air Pro review
How we tested the best air purifiers
We conducted a meticulous and replicable testing process to find the best air purifiers out there. Each air purifier was subjected to the same tests, as much as possible, in the same conditions.
We first tested the air purifier's purifying performance in "normal" conditions (a single, mid-sized room in a house with no pets). We measured how it performed with a particle counter measuring particles as small as 0.3 microns. We took air quality readings at the start and then at the 15-minute and 30-minute marks while running the machine on its lowest setting. Then, we ran the air purifier again for 30 minutes on its highest setting and measured the air quality by the end of that period. After burning matches and incense cones, we reiterated those tests to see how the machines would fare in high-particle count environments, simulating high pollution or pollen count.
We compared the performance achieved with the claims made by each purifier brand and revealed our findings in the "Performance" section of each review. To learn more, head to our page on how we test.
How to choose the best air purifier for you
The most important thing to consider when purchasing a home air purifier is what you want it to tackle. The best air purifiers can remove harmful particles, absorb odors, and even provide extra features like night lights or cooling fans. But even expensive models sometimes struggle to remove particles that cause allergens, such as pollen, dust, pet dander, and particles emitted by household chemicals.
For example, if you have pets in your home, but some members of your household suffer from allergies to pet dander, make sure you find an air purifier that’s good at removing these particles. You’ll want an air purifier that traps pollen if you have hay fever. A quick look through the product specifications and reviews will usually tell you whether your air purifier does the job you want it to do.
Think about the layout of your home, too. If you have large rooms, you’ll need an air purifier that can handle more square feet. If you have an open-plan kitchen-diner apartment, your air purifier should be able to neutralize cooking odors and absorb harmful smoke particles. Will you want to move the air purifier from room to room? Then, you’ll need a device that’s light enough to lift and move about.
Finally, consider how much you want to spend. To get a high-quality product, you should ideally spend a couple hundred dollars on an air purifier. But that doesn’t mean cheaper models can’t do the job just as effectively or that more expensive models always do a better job than their affordable counterparts.
Reviews
Whirlpool 24" Stainless Steel AI Dishwasher Review
Napoleon TravelQ PRO285 Portable Gas Grill review
Dreame L40 Ultra Robot Vacuum Cleaner and Mop review: almost hands-free cleaning
GE Profile Smart Mixer with Auto Sense review: a powerful, thorough mixer
Echo eForce DPB-2500 review: a leaf blower as a snow removal tool?
DPAS-2100 + Pro Paddle Attachment review: a new way to remove snow this winter?
Midea MAD53109APK 5.5QT Air Fryer review: a small, simple, and highly effective option
Eureka J15 Pro Ultra Robot Vacuum review: hands-free cleaning for busy families
Consider what you want your air purifier to do and what you can spend. Then, do the research, look at as many air purifiers as you can, and decide on the right model for your home. Our guide includes all the information you need to make the right decision.
What the experts say
Experts agree that air purifiers can be an effective way to improve home air quality. Timothy Carroll, from the U.S. Environment Protection Agency (EPA), says that most air purifiers have the potential to improve your home’s air.
Most portable air cleaners can filter particles from the air, and some can filter the small particles of greatest health concern (PM2.5, that is, particles smaller than 2.5 microns in diameter)."
Timothy Carroll, EPA spokesperson
However, he's quick to point out that no air purifier will eliminate all the air pollutants in a home, and most air purifiers are designed to tackle just one room or area.
Carroll says you can increase the effectiveness of your air purifier by taking a few simple steps. These include reducing or removing the sources of indoor air pollutants and ventilating where possible with clean outdoor air.
Carroll agrees that air purifiers can help reduce the symptoms of an allergy and that air purifiers can be one weapon in your armory. "Multiple studies with portable air cleaners that use a HEPA (high-efficiency particulate air) filter have found improvements in one or more allergy and/or asthma symptoms." But, he adds, "studies do not always show major improvements, and they do not show improvements in all symptoms." So, it's vital to remove the source of the allergen and use an air purifier.
Carroll also points out that many allergens, such as large dust mites, settle out of the air quickly and accumulate on surfaces. So many may never reach your air purifier in the first place. Although air purifiers can help remove particles caused by mold and help to reduce musty odors, Carroll says, "they will not resolve a mold problem. To solve a mold problem, it is necessary to get rid of the source of the moisture and clean up the mold."
Air purifier FAQs
Does an air purifier help with wildfire smoke?
If you live in an area that may suffer from air damage caused by wildfires, you could benefit from an air purifier. A HEPA filter-toting air purifier will help clean the air in your home of the potentially harmful fine particles from wildfire smoke that can get into your rooms.
Since these models are mostly made to clean the air in a single room, you may want to invest in more than one. You may also want to place the air purifier in the room you use most or spend the most time in, like your bedroom.
The severity of the wildfire, your proximity to it, and your home's ability to keep out smoke can all define the level of filtration system you may need. Certainly go for HEPA, as this offers the best filtration, but also think about that CADR number, going for a higher one even in smaller rooms if you think that smoke could be great in its amount.
Is it good to use an air purifier every day?
The answer to this question is a definitive yes. Air pollution is constant, so you are advised to leave your air filter on all day to keep ahead of that. Many models are designed to be quiet and low energy consuming, so they can be used exactly that way.
Aside from the ongoing costs of the unit and potential filter replacements, there are no other drawbacks to leaving your unit on all day. So, if the sound isn't an issue for you, then leaving it on will just mean cleaner air. This won't take anything good out of the air, for example, so it can't hurt to leave it on and running to make sure all allergens and potential toxins are removed from the air as they appear.
It is recommended that you leave your air purifier on day and night. If you switch it off, dust, dander, and allergens will build up again. Turning the unit back on forces it to work through all that build-up again, leaving you vulnerable and the machine working harder. Leaving the unit on can make smaller and more consistent cleaning easier on the purifier while keeping you safer at the same time.
Sign up to receive the latest news, reviews, buying guides and deals direct to your inbox

Joanne Lewsley is a reputable freelance writer specializing in evidence-based health and lifestyle content. With a background in journalism and extensive experience working for known brands, Joanne rigorously tests and evaluates home gadgets. Her passion for writing is complemented by her love for the outdoors and live music.
